My last post, on current imaging techniques for PSP, was kind of technical and its last paragraph promised that the next one would be something softer. But someone just sent a comment asking why I didn’t mention dopamine transporter (DaT) imaging. So I’ll defer the low-tech post and in this one I’ll explain why I omitted DaT scan from my previous post. Here’s why: It’s not useful in distinguishing PSP from its likeliest diagnostic alternatives.
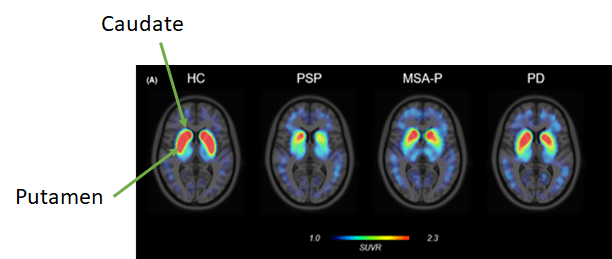
The dopamine transporters are molecules in the caudate and putamen (which together are called the striatum). See the highlighted structures in the image just below:

The brain cells bearing the DaT molecules have their cell bodies down in the substantia nigra of midbrain and send their axons up to the basal ganglia to synapse in the caudate and putamen, where they use dopamine as their neurotransmitter. In PSP, MSA, CBD, dementia with Lewy bodies and some others, those neurons are among the first to die and in Parkinson’s they’re not the first, but they’re the most important. So any imaging technique that reveals those neurons will be abnormal in all those diseases.
In the images below, the red and yellow areas represent the greatest presence of DaT molecules. The “head” of the comma-shaped thing is the caudate and the “tail” is the putamen. They’re nice and chunky in the leftmost image, labeled HC for healthy control. People with PSP, MSA-Parkinson type and Parkinson’s disease have lesser DaT signals, and the differences among those are just related to the severity of illness in those three individuals. They all have the same basic abnormality.
So, the DaT scan can quantify the severity of disease but cannot distinguish among the various neurodegenerative causes of Parkinsonism. Of course, for purposes of patient care, one can quantify PSP severity more easily, cheaply and usefully with just a history and exam.
What DaT can do, and this is its only official, FDA-approved use, is to distinguish essential tremor, where the dopamine-producing neurons are normal, from degenerative causes of tremor, where of course they’re not. Uses of the DaT scan that have not been approved by the FDA because of insufficient data are to distinguish degenerative Parkinsonism from normal-pressure hydrocephalus, drug-induced Parkinsonism, hypothyroidism and a bunch of other things that cause muscle rigidity and slow movement for reasons other than loss of the dopamine-producing neurons. But all of those things can be diagnosed in other ways.
Another difficulty with the technique is that many commonly-used neurological drugs such as antidepressants can cause false-positive DaT scans by blocking the dopamine transporter.
Bottom line: Other than to distinguish unusual cases of essential tremor from degenerative Parkinsonism, most movement disorders specialists rarely or never order DaT scans for routine patient care because they add nothing to a properly performed history, neurological exam and MRI.