When someone with PSP reports a feeling of “weak muscles” to their neurologist, the answer is typically, “yes, you’re weak, but the problem isn’t in your muscles – it’s in the messages to your muscles from your brain.” But it turns out that in PSP, muscles can be a problem, too, and that opens up some treatment potential.
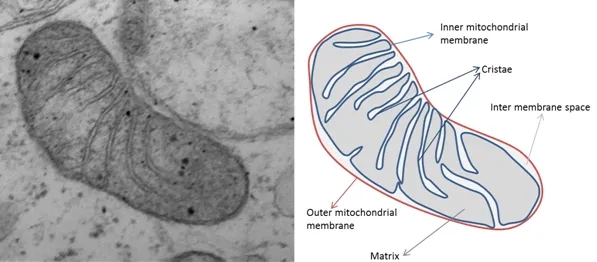
We’ve known for decades that the mitochondria aren’t working right in PSP and other neurodegenerative diseases. You’ll recall that those are the tiny factories in almost all our cells devoted to the biochemical process of respiration – that where oxygen and sugar combine to produce energy for the cell’s many functions. Besides that very important job, mitochondria are also involved in processes such as neural plasticity (the ability of brain cells to react to external influences), calcium regulation, electrical properties of the cell and synaptic transmission.
Here’s a electron microscope photo of a single mitochondrion (from this source).
What brain cells and muscle cells have in common is the need to maintain very different concentrations of potassium between themselves and the surrounding fluid (called a “gradient”), and that takes lots of energy. So, any defect in mitochondria will tend to hurt brain cells and muscle cells first and worst. In fact, childhood neurological dysfunction and muscle weakness are the two main features of a whole category of diseases caused by single-gene mutations affecting proteins used only by mitochondria.
In PSP, the mitochondrial problem is more subtle, but we don’t know exactly what it is or what causes it. Here are some strands of evidence:
- Brain cells growing in a dish that have had their own mitochondria destroyed and replaced by mitochondria isolated from blood cells of people with PSP don’t recover from various kinds of stress as well the same brain cells with replacement mitochondria from healthy people.
- Toxins damaging an important series of chemical reactions in the mitochondria called Complex I can cause a PSP-like condition in lab animals.
- Complex I and other components of mitochondria are also damaged by tau molecules with an abnormal number or location of attached phosphate molecules (“phospho-tau”), which we know occur in PSP. The net effect is excessive levels of “free radicals,” which are toxic by-products of normal respiration.
- While the most important gene mutation contributing to PSP risk is in MAPT, which encodes tau, the next-most important is PERK (protein kinase RNA-like endoplasmic reticulum kinase), which regulates the responses to stress in mitochondria.
- Coenzyme Q-10, a nutritional supplement that assists Complex I, may help some of the immediate symptoms of PSP, as shown by at least one double-blind trial.
All the above is simply background justification to suspect that muscles and not just brain should be involved in PSP. But there’s more direct evidence, too:
- Muscle weakness and fatigue are more common in PSP than in others of the same age.
- Weight loss is common in PSP and occurs early in the disease course. The same is true for both in Parkinson’s, but not as markedly.
- Grip strength is impaired in PSP. That could be a result of changes in the brain, but the duration of the muscle fiber contractions is prolonged in PSP, a sign of muscle dysfunction.
- Men (but, oddly, not women) with PSP have a reduced overall muscle mass relative to others of the same age.
- Muscle biopsy in people with PSP shows modest evidence of the same severe change in mitochondria (called “ragged red fibers”) that occur in the genetic mitochondrial diseases of childhood.
So, what’s the take-home for people with PSP?
- First, EXERCISE – including low-intensity muscle-building exercises. Discuss the details first with your neurologist or physical therapist, and probably also with your primary care physician to make sure your heart and lungs are up to the task.
- Second, HAVE HOPE that insights into the mitochondrial role in PSP will bring new treatment or neuroprotection targeted at those cellular processes in the brain. In fact, one such medication, called AMX-0035 (a combination of taurursodiol and sodium phenylbutyrate) will be entering a Phase 3 trial for PSP in the next few months. The combination under the brand name “Relyvrio” was approved last year by the FDA for Lou Gehrig disease, where there’s a similar mitochondrial problem, so I have very high hopes that the same will happen for PSP.