Everyone with a suspected diagnosis of PSP should have a brain MRI. It can find more-readily-treated things such as strokes, tumors or normal-pressure hydrocephalus. But the MRI is not all that useful in differentiating PSP in its early, diagnostically-uncertain, stages from other neurodegenerative conditions such as Parkinson’s, MSA, Alzheimer’s, CBD, dementia with Lewy bodies, and the several forms of FTD. Even the famous hummingbird sign of PSP doesn’t appear until the middle stages of the disease, by which time a neurologist can make the diagnosis by history and physical exam anyway. Besides, any disorder that causes atrophy of the midbrain will produce a hummingbird sign.
But now, researchers at the University of California, San Francisco and the Universitat Autònoma de Barcelona have used an automated system to measure the degree of atrophy of several areas of brain as seen on MRI. The system, called “FreeSurfer,” is in standard use in research requiring MRI measurements. The lead author was Ignacio Illán-Gaia and the senior author was Adam Boxer. All of their 326 subjects had been evaluated at UCSF’s Memory and Aging Center between 1994 and 2019. The diagnosis in each case was later established at autopsy – a major scientific strength of this study. Autopsy showed PSP in 68, CBD in 44, various forms of FTD in 144, Alzheimer’s in 45, and PD, MSA or DLB in only 11.
The four brain areas chosen for analysis were all previously known to atrophy in PSP: cerebral cortex, midbrain, pons and superior cerebellar peduncle. (The midbrain and pons are in the brainstem and the SCP is one of three tracts connecting the cerebellum to the rest of the brain.) They used not only the size of each, but also a previously reported index called the “magnetic resonance parkinsonism index” (MRPI), a formula involving the size of the midbrain, pons, SCP and middle cerebellar peduncle. (See note below for details.) The MRPI does very well in distinguishing PSP from PD, but has not been adequately evaluated against all possible alternative diagnoses. Actually, an updated version called “MRPI 2.0” can distinguish PSP from MSA because it takes into account atrophy of the thalamus, but it’s too new to have an automated version, so this project satisfied itself with the MRPI.
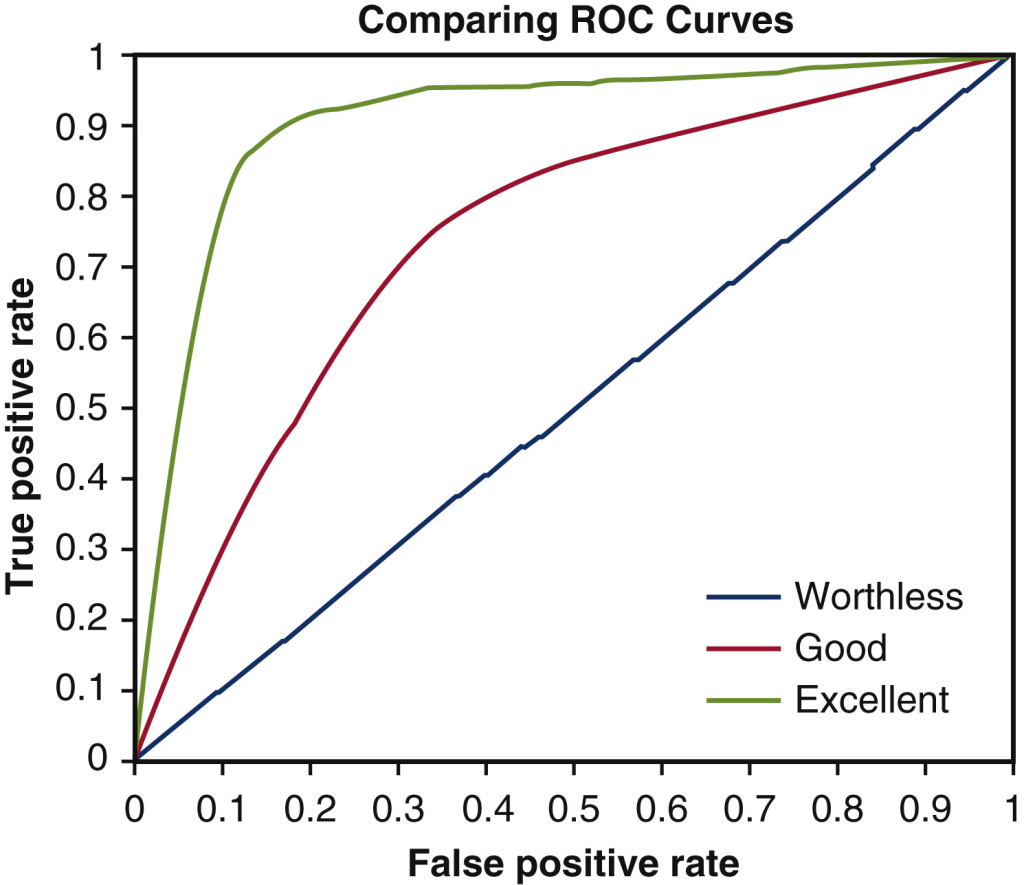
The result was that the MRPI showed an excellent ability to distinguish PSP from the other diseases as a group. The area under the receiver operating curve (AUROC; see my previous post for an explanation) was excellent: 0.90 of a possible 1.00. But the AUROC for distinguishing PSP from CBD was only moderate at 0.83. A more sophisticated statistical analysis, a “multiple logistic regression model” (MLRM), worked even better, distinguishing PSP from the others with a superb AUROC of 0.98. The CBD- vs-others comparison also benefited from the MLRM, rising to 0.86.
To put the AUROC into more-relatable terms: The AUROC of 0.98 in this case corresponds to an “accuracy” of 95%. That means that the MLRM got the diagnosis correct (i.e., PSP or not PSP) in 95% of patients. But that simple calculation can be misleading, which is why the AUROC is used by researchers.
As mentioned above, the total number of patients with PD, DLB and MSA was only 11. That’s because the study was performed at a memory center, not a movement center. While the MRPI has proven its utility in distinguishing PSP from PD, the same can’t be said for the PSP vs DLB or the PSP vs MSA comparisons. So we need more work with a statistically robust number of patients with DLB and MSA.
For an admittedly biased assessment of the importance of this study, here’s Dr. Illán-Gaia in emailed comments in response to my request for a couple of quotable blurbs:
Our study demonstrates in a large autopsy-proven cohort that combining a set of cortical and subcortical measures of cerebral atrophy could represent a powerful diagnostic tool. These measures can be obtained with a simple MRI and could be combined with other biomarkers to improve the diagnosis of patients with PSP or CBD.
More work needs to be done to ensure the translation of our method to clinical practice and we are now working to validate our results in other large multicenter studies.
Notes:
The MRPI is calculated as follows: (area of pons on mid-sagittal section / area of midbrain on midsagittal section) X (diameter of middle cerebellar peduncle on parasagittal section / diameter of superior cerebellar peduncle on coronal section).
The MRPI 2.0 multiplies the MRPI by the (maximum width of the third ventricle / maximum width of the frontal horns of the lateral ventricles).