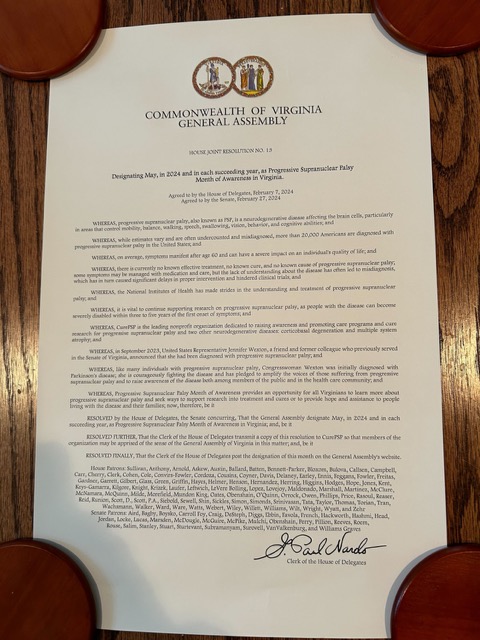
You’ll recall from my 7/4/24 post that Rep. Jennifer Wexton of Virginia announced last year that she has PSP. Below is a new press release from her office. My point relates to its final paragraph.
Wexton Marks Disability Pride Month on House Floor Using New AI Voice Model
Washington, July 25, 2024
Washington, DC — Today, Congresswoman Jennifer Wexton (D-VA) delivered a speech on the floor of the House of Representatives to recognize Disability Pride Month, celebrated each July. Wexton utilized her new AI voice model for the first time on the House floor to share how she has fought throughout her career for disability rights and accessibility issues, and how that has now become a personal fight for her since her Progressive Supranuclear Palsy (PSP) diagnosis last year.
“I hope that when people see me continuing to do all I can to keep living my life and doing this job I love as best I can, they understand and appreciate the courage, resilience, and spirit that so many Americans of differing abilities demonstrate each and every day. I hope I can be a voice — even an AI voice — for Americans facing accessibility challenges and other disabilities, because too often people only see us for that disability. And in truth we are so much more,” said Wexton.
The AI voice model was created through ElevenLabs, a software company that specializes in developing natural-sounding speech synthesis software using deep learning. The model was generated consensually using a collection of previous public speeches from Rep. Wexton provided by her team. Any additional questions about the ElevenLabs technology can be directed to press@elevenlabs.io.
More than the nominal topic of Disability Pride Month, the text mentions that she used an AI-based speech aid to deliver a speech on the floor of the House. It used audio recordings of her public speeches before PSP’s dysarthria set in to train the AI software to translate a written text into speech in her own voice, not the electronic, synthetic voice we all recognize as “computer speech.” This is important because the distinctive timbre of one’s speech provides an important emotional identifier.
This technique, relying as it does on a prepared, written text, is not suitable for ordinary two-way conversations unless you can type extremely fast. Few people with PSP can do that, even with the help of word-completion software. Besides, hardly anyone has a collection of old audio clips on which to “train” the AI software that Rep. Wexton used. An audio bank deliberately created for this purpose in an early stage of illness is one potential solution.
I wanted to review the latest on this topic, mostly to help me advise CurePSP about what sort of programs or research it might support going forward. So, I consulted my newest muse, ChatGPT. Here’s what it had to say about voice banking and other solutions for severe dysarthria:
You can bank your own voice for future use in a speech generation app in case you become disabled. Voice banking involves recording a variety of phrases and sentences while your voice is still healthy. These recordings can later be used to create a synthetic version of your voice, allowing speech generation apps to produce speech that sounds like you.
Here are the general steps to bank your voice:
Choose a Voice Banking Service: Select a service that offers voice banking. Some popular options include VocaliD, Acapela, and ModelTalker.
Record Phrases: Follow the service’s instructions to record a set of phrases and sentences. The more you record, the better the quality of the synthesized voice.
Submit Recordings: Upload your recordings to the voice banking service.
Voice Synthesis: The service will process your recordings and create a synthetic version of your voice.
Integration with Speech Generation App: Once your synthetic voice is ready, it can be integrated into a speech generation app. This allows you to communicate using your own voice even if you lose the ability to speak naturally.
Voice banking is a proactive step that can significantly improve the quality of life for individuals facing conditions that may affect their ability to speak.
Alternatives to voice banking?
If voice banking is not a suitable option for you, there are several alternatives that can help with communication if you become disabled. Here are a few options:
1. Voice Cloning
Voice cloning uses advanced AI to create a synthetic version of your voice with fewer recordings. Services like Respeecher and Descript can create high-quality voice models from a limited amount of audio data.
2. Text-to-Speech (TTS) with Customization
Text-to-speech technology can be customized with different voices, accents, and tones. Some TTS systems allow you to adjust parameters to make the voice sound closer to your own. Popular TTS engines include:
Amazon Polly
Google Text-to-Speech
Microsoft Azure Speech Service
3. Pre-Recorded Messages
You can record common phrases and sentences that you might need. These recordings can be played back as needed. Devices like the GoTalk series or AAC (Augmentative and Alternative Communication) devices often support this feature.
4. Alternative and Augmentative Communication (AAC) Devices
AAC devices and apps provide various ways to communicate through symbols, text, and synthetic speech. Examples include:
Tobii Dynavox
Proloquo2Go
TouchChat
5. Predictive Text Apps
Predictive text apps can assist in quicker communication by predicting the words and phrases you are likely to use. These apps learn from your typing habits to offer more accurate suggestions. Notable apps include:
SwiftKey
Gboard
6. Communication Boards and Books
Low-tech options such as communication boards or books with pictures, symbols, or letters can be very effective, especially in environments where technology might not be available.
7. Eye-Tracking Technology
For individuals with severe physical disabilities, eye-tracking technology allows communication through eye movements. Devices like the Tobii Eye Tracker can be used to control computers and AAC software.
8. Sign Language and Gestures
If you retain some physical ability, learning sign language or using a system of personalized gestures can be an effective way to communicate.
Each of these alternatives offers different advantages depending on your specific needs and circumstances. Exploring these options can help you find the most effective means of communication in the event of disability.
Now back to human me.
It goes without saying that these solutions have to be tailored to the individual – no easy task considering that the disease itself worsens with time. Another complication is that many of the techniques require manual dexterity or eye movement control beyond the abilities of many people with PSP. (It also goes without saying that anything from ChatGPT can be incomplete or even wrong.)
Medicare pays most of the cost of some of these things if there’s a doctor’s prescription. Discuss with a speech pathologist, which you should be doing anyway for general PSP-related speech and swallowing issues.
If you consider me your PSP muse, whose mine? Now I know.