Decades ago, the discovery that specific proteins aggregated in the brain cells of specific neurodegenerative diseases was a major advance. But like so many other scientific breakthroughs, it created another question: Why are there so many different clinical pictures among different people with the same neurodegenerative disease (like PSP) despite the fact that they all host the same aggregating protein (in this case, tau)? The ability of abnormal tau to “seed” the disease process into previously healthy brain areas is at the root of the disease process, but we’ve had scant clue as to how that works, exactly.
For PSP, the most important clinical variable is the eight subtypes (PSP-Richardson’s syndrome vs PSP-Parkinsonism vs PSP-progressive gait freezing, etc), and slightly less variable features are the onset age and rate of progression. In the past year or two, it’s become clear that the different subtypes tend to emphasize different areas of the brain, but that doesn’t explain why two people with the same subtype can have different onset ages and rates of progression.
This mystery became even more mysterious recently when a new electron microscopy technique called “cryo-EM” proved able to visualize individual protein molecules. It showed that for everyone with a given disease, the protein for that disease had the same misfolded shape. In other words, the tau molecule assumes the same rigid squiggle in everyone with PSP, a different rigid squiggle in everyone with Alzheimer’s, yet another in everyone with corticobasal degeneration, and so on. But that raised the question as to the reason for the variability among patients of the PSP onset age and rate of progression.
Now, researchers at the Rossy Centre, a facility dedicated solely to PSP research at the University of Toronto, have found new evidence supporting the old idea that the key may be in the “oligomers” or “high-molecular weight tau” or “HMW tau.” These are stacks of tau protein molecules small enough to remain dissolved in the brain’s fluids, as opposed to single molecules or the large, insoluble neurofibrillary tangles visible through a conventional microscope.
The top-line result was that the patients with more rapidly-progressive PSP and brain regions with the worst damage had higher levels of HMW tau. In a tour-de-force of lab experiments, the Toronto researchers also showed that:
- HMW tau was more resistant to the brain’s mechanism for breaking down such protein clusters.
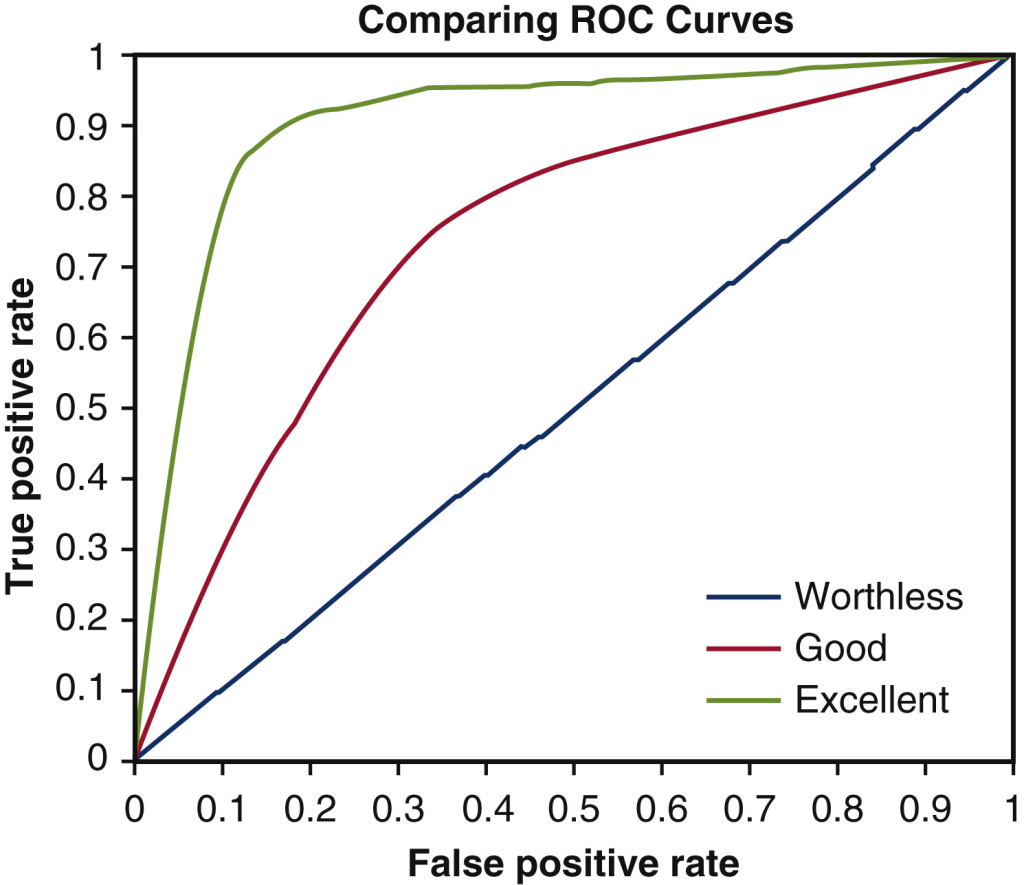
- The study’s 25 PSP patients could be divided into high-, medium- and low-seeders based on the speed with which their tau converted healthy tau to their own misfolded form.
- Tau with phosphate groups attached to amino acids 202 and 205 were least likely to form the HMW tau clusters.
- The pattern of production of proteins (i.e., the “proteomics”) in the brain areas rich in HMW tau showed disruption of the brain’s adaptive immune system and two other cellular systems previously known to be related to neurodegeneration.
The importance of all this is that we now have a more specific idea of the structure of the most toxic form of tau aggregates and that boosting the brain’s adaptive immune system with medication could discourage the seeding of misfolded tau into healthy cells.
The study’s first author, Dr. Ivan Martinez-Valbuena, published an editorial in the journal Brain Pathology explaining all this in language that non-specialist scientists can understand.
The research paper itself is posted by the authors in bioRxiv (“bio-archive”) an on-line, open-access website for articles awaiting word from the peer-review process at a conventional journal. Its senior author is Dr. Gabor Kovacs, one of the world’s leading neuropathologists in the field of neurodegenerative diseases.