My last post was about AADvac1, one of the three neuroprotective drugs set to inaugurate the PSP Trial Platform (PTP) later this year. Today’s post is about the second drug, AZP-2006. The third drug has not yet been finalized, but at a conference in London last week, Dr. Adam Boxer, the leader of the PTP, said it will be revealed soon.
The PTP trials are all Phase 2a, meaning that they’re designed primarily to assess safety and tolerability. However, they do include enough patients, typically about 100 or 200, to detect drug benefit if any indeed exists. The benefit would be in the form of slowing of the rate of progression of PSP as measured by a newly abridged version of the PSP Rating Scale. The PTP will recruit one placebo group to serve as a comparator for all three active-drug groups.
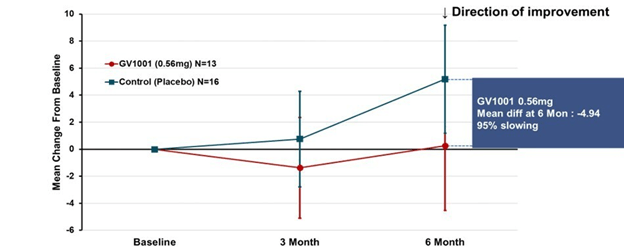
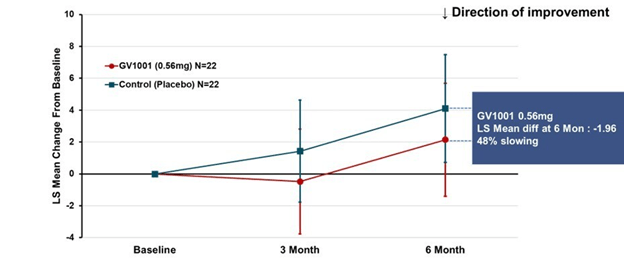
An unpublished Phase 1 PSP trial in 36 people with no placebo group found a 31% slowing of the PSP Rating Scale progression relative to placebo groups in previous PSP drug trials. I hasten to add that comparing the results of active drug in an uncontrolled study to the placebo group in a completely different study is a minefield. So, let’s not jump to conclusions about the efficacy of this drug. All we can say is that the result justifies further investment and study.
That said, I’ll point out that in placebo-controlled Phase 2b and Phase 3 trials, a slowing of 20% or 25% relative to the placebo group is often considered adequate to consider the drug for approval.
AZP-2006 is administered as an oral liquid, which is more convenient than the intravenous, subcutaneous or intrathecal (into the spinal fluid) routes of some of the other current experimental PSP drugs. But of course, oral liquids can be a major issue for those with PSP, though it seemed not to cause any dropouts or serious adverse effects among the 36 patients in the Phase 1 trial. I don’t know if the AZP-2006 oral solution is compatible with the commonly used gelatin- or starch-based drink thickeners. The PTP trial will be confined to patients in early to moderates stages of disability, without the more pronounced swallowing difficulty of the later stages.
Nerd Alert: The main mechanism of action of AZP-2006 is at the lysosomes, one of the cell’s garbage disposal mechanisms, where it acts specifically at the lysosome’s prosaposin and progranulin pathways. Prosaposin is the metabolic precursor (a “parent molecule” cleaved by enzymes to produce the active molecule) of the saposins, a group of proteins required for the normal breakdown of various types of lipids that are worn out or over-produced or defective from the start. Progranulin is the precursor, as you’d guess, of granulin, which, like saposin, is involved in function of the lysosomes. But progranulin addresses disposal of proteins, not lipids. In mouse experiments, the drug also enhances the production of progranulin, mitigates the abnormal inflammatory activity in tauopathy, reduces tau aggregation, and stimulates the growth or maintenance brain cell connections. The company has not published or otherwise released details of the mouse work and if they know the details of these mechanisms of action, they’re keeping them secret for now.
One hereditary type of familial frontotemporal dementia where TDP-43 is the mis-aggregating protein is caused by mutations in the progranulin gene. However, progranulin mutations seem not to be related to PSP.
AZP-2006 was developed by Alzprotect, a company headquartered in Lille, France that was started in 2007 and has no approved drugs as yet. Here’s a page from the company’s website. It includes a nice video with an artist’s conception (or a PR consultant’s dream) of how the drug works.
AZP-2006 may be the most likely to succeed among the currently announced anti-PSP candidates in or nearing clinical trials. That’s because it addresses multiple important cellular abnormalities simultaneously (see the Nerd Alert above), something that many of the experts feel will be sine qua non for any successful PSP neuroprotective drug.