A bit of encouraging news this week.
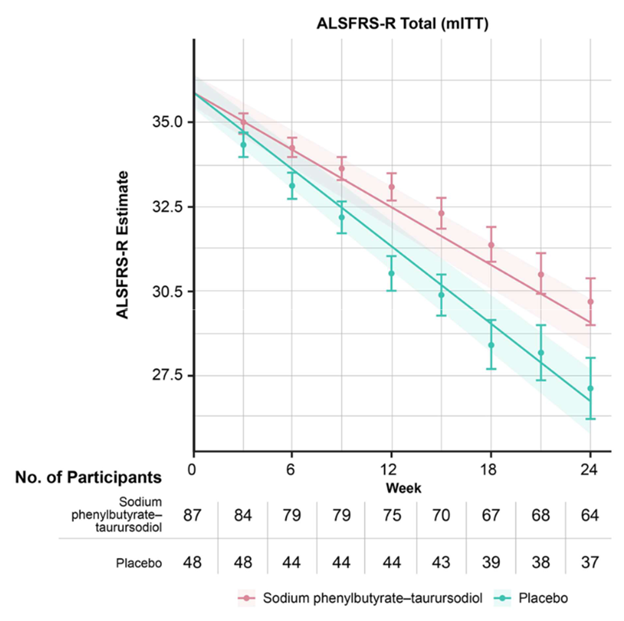
As explained in my post of March 10 (“No panacea”), the trial drug Relyvrio was found not to help amyotrophic lateral sclerosis. This despite positive results last year from a smaller trial that had prompted the FDA to provisionally approve the drug for ALS. After this new result, the company, Amylyx, withdrew the drug from the market. However, an ongoing trial of Relyvrio for PSP will continue.
Relyvrio is also being tested not only in PSP, but also in patients with Wolfram syndrome. In case you haven’t heard of this genetic condition that’s about 2% as common as PSP, it causes a combination of insulin-requiring diabetes, excessive urine production (“diabetes insipidus”), blindness from degeneration of the optic nerve, and deafness, along with neurological issues such as seizures, mild cognitive loss and loss of respiratory drive. Wolfram syndrome starts at an average age of only six, with a range of six weeks to 19 years. Sufferers die by age 40, usually from complications of diabetes or from respiratory failure. A sad picture, indeed.
So what’s the encouraging news? Amylyx issued a press release on April 10 (three days ago) reporting interim results halfway through their 48-week, 12-patient, unblinded trial of Relyvrio in adults with Wolfram syndrome. Eight of the 12 patients had completed the trial by that date. The levels of a protein involved in the synthesis of insulin, called C-peptide increased and do so more promptly after a meal. C-peptide is a standard test in medical practice to assess the severity of diabetes. There was also a small improvement or lack of worsening in hemoglobin A1C; the fraction of the day in the normal blood glucose range; visual acuity as measured by a standard wall chart; and global impressions by the doctor and patient (separately) of how well things are going overall. Over 24 weeks, these patients would have been expected to worsen, on average, not to improve or stabilize as these eight patients apparently did.
Keep in mind that the comparator wasn’t a placebo group, but “historical controls,” meaning patients from previous research or from the study doctors’ regular practice. (Unfortunately, the company’s press release didn’t say just how much people with with Wolfram syndrome would be expected worsen in these measures over 24 weeks.) This opens the possibility that the patients in the study might simply have taken better care of themselves, knowing they were being tested in the trial. Another possibility is that the doctors themselves fell victim to their hopes for the patients, providing more aggressive general management of their symptoms during the trial. That’s why we do double-blind trials. If the current trial gives favorable results after all 12 patients have completed the 48 weeks, then presumably Amylyx will move to a larger and double-blind trial.
This is, provisionally, slightly good news for people with Wolfram syndrome, but what about PSP? Both diseases involve abnormalities in the “unfolded protein response” (UFR) in the brain cells’ endoplasmic reticulum (ER). After amino acids are strung together in the cell’s nucleus to make proteins, they’re transported to the ER, where they’re folded into the patterns they need to do their jobs. In both Wolfram syndrome and PSP, there’s an abnormal overactivity of the UFR, and Relyvrio inhibits it.
To date, we know of 11 genes that each confers a slightly increased risk of developing PSP. The most important is the MAPT gene, which encodes the tau protein. The next-most important is a gene called EIF2AK3, which encodes a protein called PERK, which is an important part of the unfolded protein response.
So let’s await the final results in this early-phase trial of Relyvrio in Wolfram syndrome. More to the point, let’s await results from the 600-participant, double-blind trial of Relyvrio in PSP, which has only just started recruiting and should end in mid-2027.
Disclosure: I’m a paid consultant for Amylyx. I assisted in the design of their PSP trial and in teaching the study doctors how to properly use the PSP Rating Scale. I have no stock in the company or any other financial interest in their commercial success.