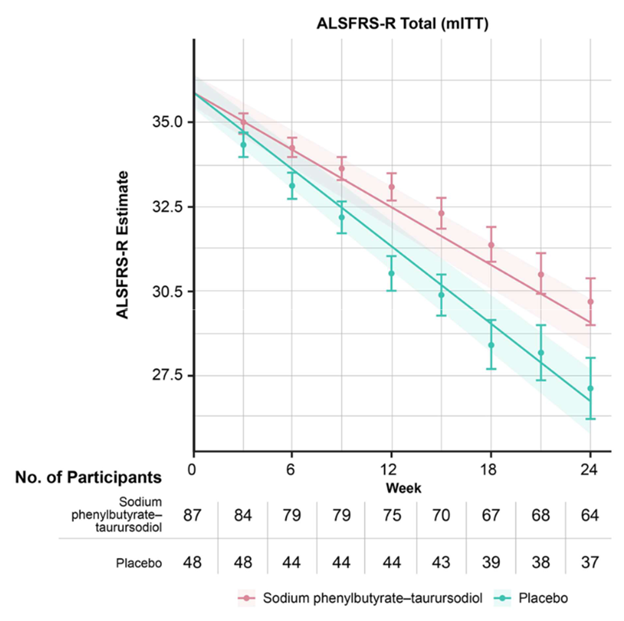
In case you missed the front-page story three days ago (3/8/24) in The New York Times, the drug Relyvrio has failed to show benefit in a large (664 participants), Phase 3 trial in amyotrophic lateral sclerosis. The drug did appear to show benefit in a much smaller (137 participants) Phase 2 ALS trial in 2020 and was provisionally approved for sale by the FDA on the strength of that result. Now, the drug company, Amylyx, may have to discontinue marketing the drug for ALS.
Why is this relevant to PSP? Because four months ago Amylyx initiated a 600-participant Phase 3 trial of Relyvrio for PSP. It’s called “ORION.” So far, recruitment has begun at only a handful of sites, all in the US, with plans to expand into Europe and Japan over the coming months. The FDA’s permission to start ORION without a Phase 1 or 2 in PSP was based in part on the success of the drug in the Phase 2 ALS trial. See my post of February 29 for details.
Amylyx is also testing Relyvrio in people with Alzheimer’s disease, where a Phase 2 trial has demonstrated adequate safety and tolerability. I have no information on a Phase 3 in AD.
The question now is whether the ORION trial in PSP will continue. So far, there’s been only one business day since the ALS news, and I’m not sure if the top brass at Amylyx — or the company’s sources of financing — have yet decided. But the Times article reported that the FDA approved Relyvrio for ALS only after Amylyx agreed to withdraw the drug if the Phase 3 trial showed no benefit. Furthermore, right after the ALS trial news hit, the stock price of Amylyx dropped from $19 to $3 and stayed about there. Stock markets usually know how this sort of news is likely to play out. Relyvrio is Amylyx’s only marketed product but they do have other drugs in the development pipeline.
The mechanism of action of Relyvrio addresses issues important to both disorders, which suggests that if it failed in one, it could well fail in the other. But we don’t really understand the pathogenesis of either disease well enough to know if PSP might respond when ALS did not.
Meanwhile, if you were planning to try to enroll in the ORION trial, I’d advise you not to change your plans. The ALS trial showed no important toxicity, at least in people with ALS, and you wouldn’t want to lose your potential spot at the study site because you delayed enrolling until definite information on the future of the ORION trial became available. When other trials in PSP start enrolling, that advice could change, of course.
(I’ll repeat the disclosure I made in my 3/8/24 post: I’m a paid consultant for Amylyx, advising them on design of the ORION trial and training the participating neurologists on proper administration of the PSP Rating Scale. But I have no stock in the company nor other financial interest in the drug’s success.)